When workplace injuries happen, achieving the best medical outcomes requires “Employee Advocacy”, as discussed in Part 2 of this six-part series. Better medical outcomes also require active engagement from key players, like injured workers, employers and medical providers.
For injured workers, active engagement means:
- Timely reporting of accidents and injuries –
- within a specified timeframe,
- clearly communicated in advance to the employee,
- triggered by employee knowledge of the accident or injury,
- subject to a good cause exception
- administered by a fiduciary in the best interests of the injured worker.
Timely reporting results in faster medical care and safer working conditions for co-workers.
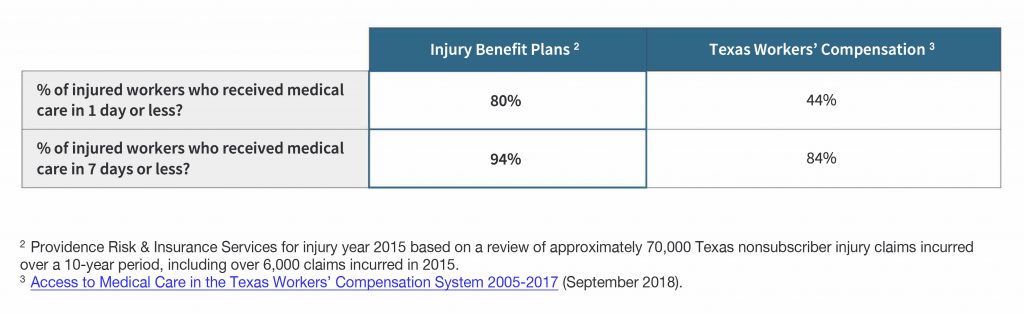
- Seek prompt medical attention from an approved provider. Multi-location medical clinics seem to be filling up with nurse practitioners, physician assistants, and temporary employee physicians, and have few (if any) medical doctors with occupational medicine training. These non-physician providers frequently punt difficult injury claims. They may be referred to other “network providers”, some of whom are well-known for preying upon injured workers that lack education or have language barriers. On the other hand, workers covered by Texas injury benefit programs are more likely to gain access to the best medical providers, including many that don’t accept workers’ compensation patients. Prompt medical treatment from quality providers makes a huge impact on medical outcomes:
This same Texas Department of Insurance report says delayed initial care is correlated with higher total medical costs. For example, Texas workers’ compensation claims with greater than seven days delay in initial medical care had on average 39 percent higher medical costs in the first 6 months after injury.
- Follow doctor’s orders. Immediate access to quality medical providers (at no fee or cost whatsoever to the injured worker) comes with a reasonable expectation for the worker to follow doctors’ orders – or pursue reasonable second opinion procedures detailed in the benefit plan, as required by federal law.
- Return to work. Unless there is an appeal or second opinion request from the injured worker, return to work is reasonably required when a physician releases the employee to full or modified duty. Returning to work at an appropriate time is well-known to promote better medical outcomes.
For employers, active engagement means:
- Communication. Don’t wait until the injury occurs! Injured workers can’t be held accountable for rules they don’t know about or understand. Common sense and applicable laws require simple, personal communications from Texas injury benefit programs that help employees know how to timely report claims, understand available benefits, and know where to obtain medical care. This helps build employee morale and a culture of caring before an injury ever occurs.
- Well-Established Benefit Claim Procedures. Federal laws require almost every employer-sponsored benefit plan (including 401k, group health and all Texas injury benefit programs) to establish reasonable procedures for administration of benefits in the best interests of covered employees and beneficiaries. The U.S. Supreme Court has, for decades, said these rules (first developed in 1974) provide administrative safeguards for a full and fair review of benefit claims, including criteria for initial benefit determinations, appeals and access to state and federal courts. Regulations also prohibit final, binding arbitration of benefit disputes. Employers failing to comply with these laws can face large monetary penalties and enforcement by the U.S. Department of Labor.
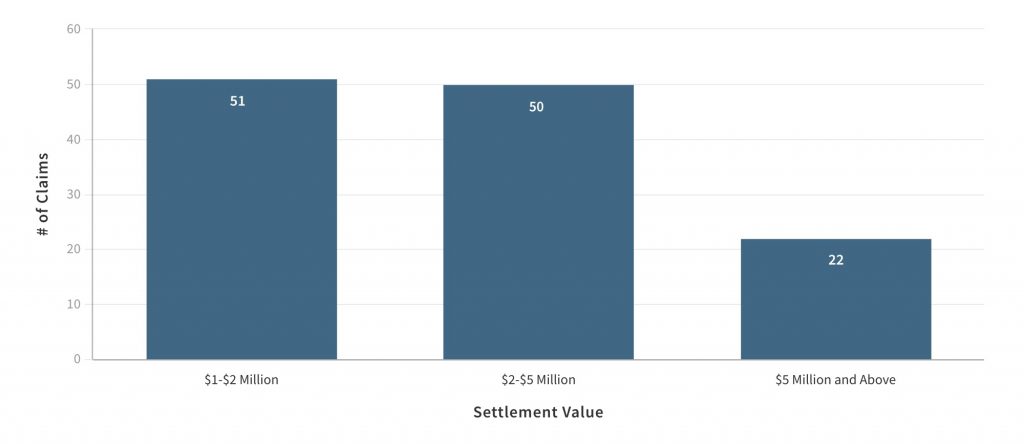
- Negligence Liability. Every employer failing to provide safety and care for their workers eventually pays the price through reduced productivity, higher insurance premiums or other increased costs of doing business. They may also be held accountable by the U.S. Occupational Health and Safety Administration (OSHA). But Texas employers with no workers’ compensation coverage are also exposed to negligence liability claims by injured workers. The “Exclusive Remedy” rule does not apply! They are exposed to lawsuits for:
- Actual damages – including any unpaid medical expenses and the employee’s lost wages, loss of earning capacity, other mental or physical damage, and pain and suffering;
- Punitive damages; and
- Attorneys’ fees.
The Texas Labor Code also strips these employers of defenses based on the worker’s assumption of risk, contributory (or comparative) negligence, or negligence of a fellow employee. Such lawsuits have developed a deep body of case law and an experienced group of attorneys representing employers and injured workers.
This reality has been a powerful force for good, commonly resulting in increased employer investments in job training, safety and return-to-work programs. It even leads some less conscientious employers to support “Employee Advocacy” and voluntarily commit in writing to pay quality injury benefits in the hopes of avoiding negligence liability lawsuits.
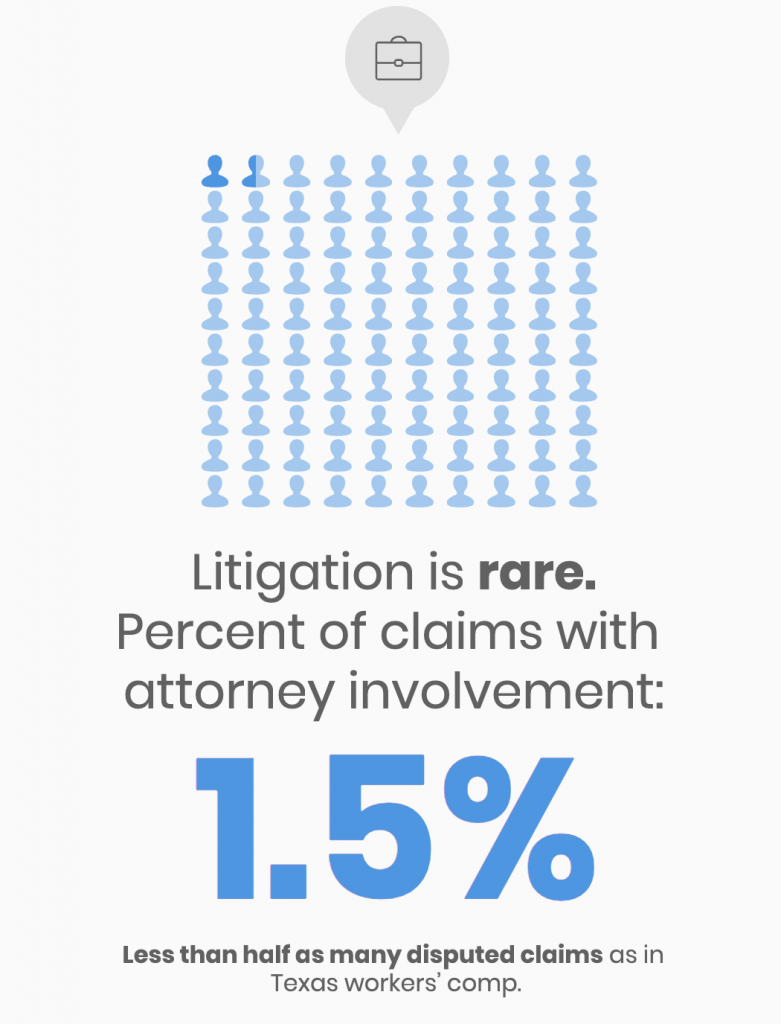
But make no mistake, exposure to negligence liability claims is real:
For medical providers, active engagement means:
- Records Review. Paying attention to both injured worker complaints and past medical records.
- Considering Medical Necessity. Doing diagnostic tests, providing injections and performing surgeries, when medically necessary. But consideration must be given to evidence-based guidelines that discourage low-value testing that is often physically or psychologically harmful, as well as unnecessary injections and surgeries that can prolong the injured worker’s pain and recovery and reduce injured worker satisfaction.
- No Opioid Abuse. Steering away from opioid narcotic drugs that commonly result in addiction and more time off work. Although Texas was the first state to begin reigning in abuse of addictive opioids and compounded drugs in workers’ compensation, this has never been a significant issue under Texas injury benefit programs due to requirements for evidence-based practice among approved medical providers.
- Approvals to Transfer Care. Pre-approval of referrals to the best available medical providers, and no referrals to physician‐owned pharmacies.
- Supporting Return to Work. Reviewing the injured employee’s job description and the requirements of any available modified duty work. Diagnosis and treatment are then better informed and work can be used, where appropriate, as a treatment modality.
Great physicians don’t hesitate to work within such reasonable standards of engagement in an environment that simplifies paperwork, streamlines approval processes, and results in a fast and fair payment for services.
Texas injury benefit programs were invented out of necessity. Thirty years later, common sense requirements and active engagement from injured workers, employers and medical providers continue to deliver better medical outcomes.